15 December, 2022
A miniaturized plasmonic spectrometer that creates a rainbow pattern that shifts in the presence of a chemical or biological sample has been developed. Crucially, these spectral shifts can be observed in a standard optical microscope.
For a beam of light to be able to interact with its surroundings, the smallest length scale is roughly equivalent to half of its wavelength. It is this principle that sets the fundamental restriction on the maximum resolution imaging optics, such as microscopes or spectrometers, can achieve. But this limit can be surpassed using plasmonics.
Plasmonic devices use nanoscale patterns to induce strong coupling between light and electrons at the surface of a metal and create so-called plasmons. Plasmons can be confined on subwavelength spatial scales and significantly enhance the strength of light-matter interactions. The former enables superresolution imaging, while the latter can be harnessed in sensitive sensors.
Qiaoqiang Gan from KAUST, together with co-workers from The State University of New York and Northeastern University in the United States, fabricated nanostrips of gold on a silica wafer.
The width and separation of the strips slowly increased across the device. This meant that light of different colors plasmonically coupled to distinct spatial regions on the chip. For example, the location of the red light was separated by approximately 50 micrometers from where blue light was trapped. “Importantly, a spatial displacement of the resonant pattern of just 35 nm was resolved by a 4× microscope system,” explains Gan. “That is equivalent to a distance of about 2.50 micrometers with 650-nanometer wavelength light.”
This concept is useful for biosensing applications because the effect is sensitive to the refractive index of any fluid on the surface. This again was made evident by a shift in where the light localized.
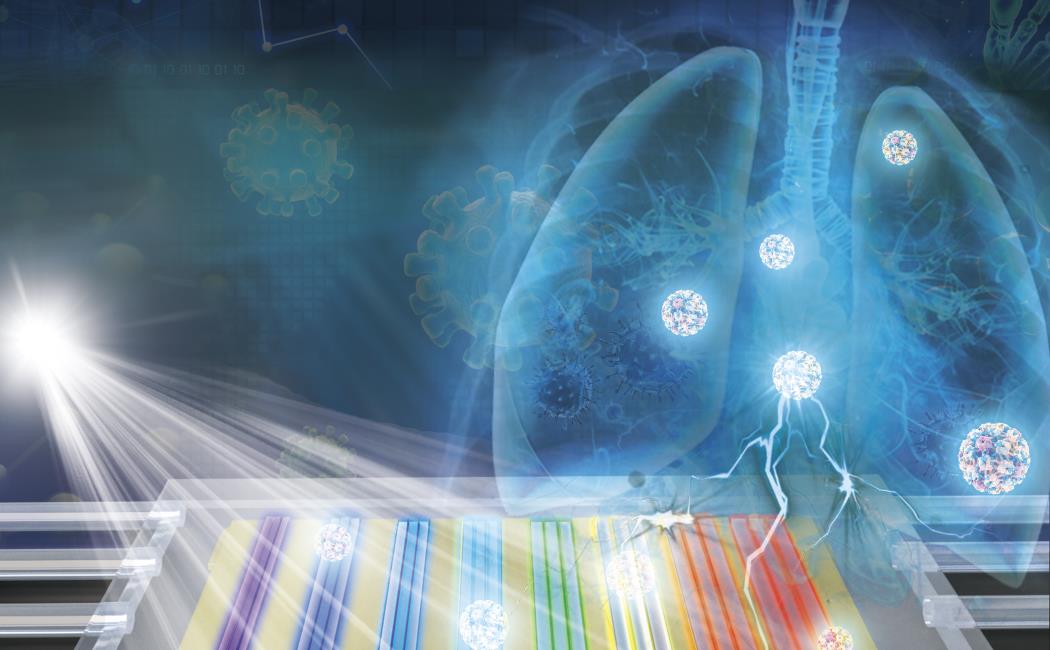
To demonstrate this idea, Gan and the team passed across their chip exosomes, a type of nanoparticle extracted from human blood, with a protein known as EGFR (exosomal epidermal growth factor receptor), which is a known indicator for lung cancer. They were able to optically detect concentrations down to 1.92 billion exosomes per milliliter.
This was sufficient to clearly differentiate between three serum samples from healthy patients and three from patients with non-small-cell lung cancer, thereby successfully demonstrating the chip’s suitability for point-of-care cancer diagnostics. “The next step is to integrate this chip with a smartphone microscope to demonstrate a portable and high-performance sensing system,” says Gan.